Nursing diagnosis for macular degeneration plays a pivotal role in guiding patient care and optimizing outcomes. Macular degeneration, a leading cause of vision impairment, affects millions worldwide, necessitating a comprehensive approach to its management.
This article delves into the intricacies of nursing diagnosis for macular degeneration, exploring the clinical manifestations, risk factors, and evidence-based interventions to improve patient outcomes. By understanding the complexities of this condition, nurses can provide tailored care that empowers individuals to maintain their independence and quality of life.
Definition and Overview
Macular degeneration is a progressive eye condition that affects the macula, the central part of the retina responsible for sharp, central vision. It is the leading cause of irreversible vision loss in people over 50 years old.
According to the World Health Organization, an estimated 196 million people worldwide have age-related macular degeneration (AMD), the most common type of macular degeneration. AMD is more prevalent in developed countries, with an estimated 11 million cases in the United States alone.
Other types of macular degeneration include Stargardt disease, a rare inherited condition that affects children and young adults, and cone-rod dystrophy, a group of inherited conditions that affect both cone and rod cells in the retina.
Nursing Assessment
Nurses play a vital role in assessing patients with macular degeneration. Signs and symptoms of the condition may include:
- Blurred central vision
- Difficulty reading or recognizing faces
- Dark spots or gaps in the central vision
- Distorted vision
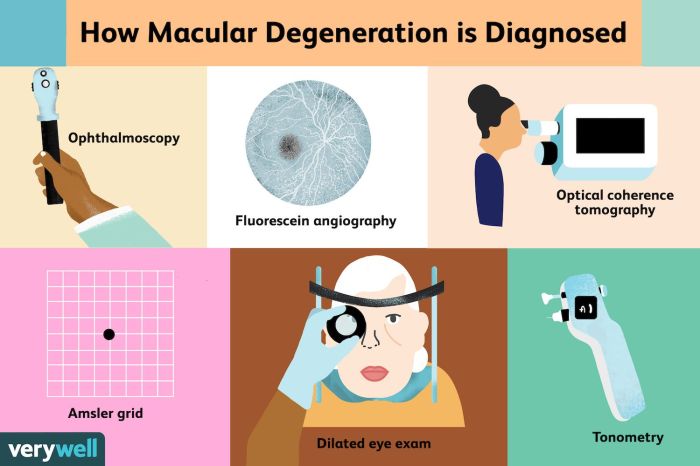
A comprehensive nursing assessment includes visual acuity testing, fundus examination, and Amsler grid testing. Patient history and risk factors, such as age, smoking, and family history, are also important to consider.
Nursing Diagnoses
Common nursing diagnoses associated with macular degeneration include:
- Impaired vision
- Sensory-perceptual alterations
- Risk for falls
Rationale for Impaired Vision:Macular degeneration damages the macula, resulting in decreased central vision and difficulty with activities that require detailed vision, such as reading, driving, and recognizing faces.
Rationale for Sensory-Perceptual Alterations:Macular degeneration can alter the perception of light, color, and depth, leading to difficulties with balance and coordination.
Rationale for Risk for Falls:Impaired vision and sensory-perceptual alterations increase the risk of falls, particularly in older adults.
Nursing Interventions
A nursing care plan for a patient with macular degeneration may include interventions to:
- Improve visual function
- Promote independence
- Prevent complications
Interventions to Improve Visual Function:
- Provide low-vision aids, such as magnifying glasses and telescopes
- Refer to low-vision rehabilitation services
- Educate patients on adaptive techniques for daily activities
Interventions to Promote Independence:
- Assist with activities of daily living, such as dressing, bathing, and cooking
- Provide orientation and mobility training
- Modify the home environment to improve safety and accessibility
Interventions to Prevent Complications:
- Monitor for signs of infection or inflammation
- Administer medications as prescribed, such as anti-VEGF drugs or corticosteroids
- Educate patients on the importance of regular eye exams and follow-up care
Questions and Answers: Nursing Diagnosis For Macular Degeneration
What are the common nursing diagnoses associated with macular degeneration?
Nursing diagnoses commonly associated with macular degeneration include impaired vision, sensory-perceptual alterations, and risk for falls.
How can nurses improve visual function in patients with macular degeneration?
Nurses can improve visual function in patients with macular degeneration through interventions such as low-vision rehabilitation, assistive devices, and medication management.
What is the importance of patient education in managing macular degeneration?
Patient education is crucial in managing macular degeneration as it empowers individuals to understand their condition, adhere to treatment plans, and make informed decisions about their care.